Former Airman 1st Class David James was fading fast on the ventilator.
Doctors with the Department of Veterans Affairs had twice asked his wife, Patty, to sign the DNR papers: Do Not Resuscitate.
Twice, Patty James refused. "My husband is a fighter," she told the doctors.
As a last resort, doctors administered to James the anti-inflammatory tocilizumab, one of the experimental drugs approved for use by the U.S. Food and Drug Administration in an effort to find a safe and reliable therapeutic for the virus.
James would become the very first case of a veteran on the ventilator to recover from COVID-19 at the Louis B. Stokes Veterans Affairs Medical Center (VAMC) in Cleveland, according to the Department of Veterans Affairs.
James was one of three recovered veterans and the wife of a recovered veteran who spoke with Military.com this month. Hailing from different parts of the country, their treatments and experiences varied; some still face painful and taxing aftereffects of the virus.
All four veterans are over age 65 and have underlying conditions that may have made them more susceptible to COVID-19.
All had little memory of being on a ventilator, and all gave high praise to the doctors, nurses and staff at the VAMCs for giving them a new lease on life -- in a pandemic that the VA and the nation's entire health care system have struggled to contain.
James is from Cleveland; former Marine Master Gunnery Sgt. Jim Warehime was treated at the Jack C. Montgomery VAMC in Muskogee, Oklahoma; former Air Force Tech Sgt. Robert Colleton was at the Overton Brooks VAMC in Shreveport, Louisiana, an area particularly hard-hit by the virus; and former Army Sgt. Mike Bolnick was at the Albany Stratton VAMC in Albany, N.Y.
They are now listed among the 24,232 "convalescent cases" of novel coronavirus, out of 34,995 total cases of COVID-19 tracked by the VA as of July 24.
Working to Treat the Virus
Since the pandemic started, the VA has reported a total of 1,965 patient deaths from the virus, which had taken the lives of a total of 144,780 Americans nationwide as of July 24, according to the Johns Hopkins University Coronavirus Resource Center.
While James was treated with tocilizumab, Warehime received "convalescent plasma," or plasma donated by a recovered COVID-19 patient; Bolnick and Colleton simply awoke from induced comas while under care at the VA.
With approval from FDA, the VA has participated in a number of industry-sponsored studies of promising medications, such as remdesivir, and including tocilizumab with Hoffmann-La Roche AG pharmaceuticals, and sarilumab, an anti-arthritic drug, with Regeneron Pharmaceuticals.
"Both drugs are used in arthritis care and block an inflammatory protein known as IL-6," according to the VA.
Clinicians at Yale New Haven Hospital have also reported promising results from the use of tocilizumab with patients severely ill with COVID-19.
In the June 15 edition of the medical journal "Chest," the Yale clinician-researchers said that patients treated with tocilizumab showed "higher than expected" survival rates but added that "randomized trials must confirm these findings."

The VA and the FDA have also issued cautionary notes on some of the promising initial results in the use of convalescent plasma to treat COVID-19.
On May 1, the VA announced that it was participating with the Mayo Clinic in studies on whether antibodies in the blood of patients who recovered from COVID-19 can help those who are still suffering from the virus.
The VA said that more than 60 of the VA's hospitals and clinics were prepared to perform the plasma transfusions for COVID-19 patients.
In a July 13 conference call with reporters, Janet Woodcock, director of the Center for Drug Evaluation and Research at the FDA, said "there's a strong possibility that convalescent plasma is helpful," but "we still don't know for sure if it works and those studies are being done as we speak."
The statistics publicized by VA show that nearly 70% of all cases, which include veterans, staff and other VA employees, have resulted in recovery; nearly 6% of all tracked cases have resulted in death, a rate almost double that within the U.S. population as a whole. Each veteran who spoke with Military.com -- and Ginger Warehime, who spoke on behalf of her still-recovering husband -- described their own survival as nothing short of a miracle.
'Miracle' For Master Guns
Jim and Ginger Warehime, of Bartlesville, Oklahoma, were high school sweethearts who married after he joined the Marine Corps in 1966.
In 1968, he was with the 26th Marine Regiment during the long siege of Khe Sanh, where he would receive the Purple Heart. Ginger waited and worried at home, unable to see him or speak with him.
Decades later, his battle with the virus would leave her with similar feelings of separation.
"It was just like Vietnam, not being able to see him -- that's what it felt like," she said. "[But] if I could make it through Vietnam with him, I could make it through anything."
Ginger, who spoke for Jim during an interview last Tuesday, said her husband had been having issues with his balance and last September fell and hit his head. He also had five back surgeries since leaving the Marine Corps, she said.
In April, he had difficulty standing up and had lost his sense of taste, Ginger said. He initially tested negative for COVID-19, but later tests came back positive.
They went to the emergency room in Bartlesville, Okla., but she kept in touch with the VA, and he was transferred to the Jack C. Montgomery VAMC in Muskogee.
"From that moment on, our lives changed," Ginger said. "Anytime we needed something, they jumped on it. They were the most generous, kind people we ever dealt with."
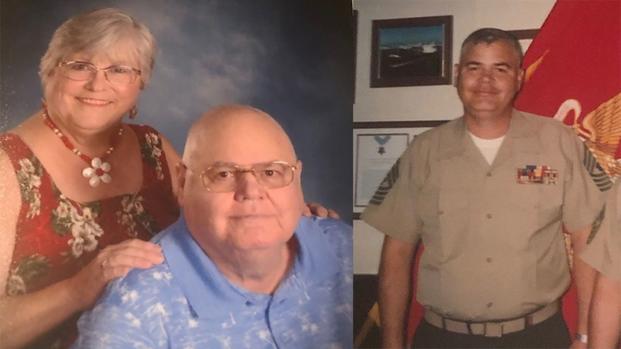
He had always been reluctant to go to the VA, Ginger said: "We had insurance, but Jim thought there were probably a lot of other veterans who needed it more."
She's still not quite sure how it happened, but Jim was approved for the use of convalescent plasma donated by a recovered COVID-19 patient.
He received the plasma May 5, and Ginger recalled the time two days later when the doctors and nurses hooked her up on a call to Jim's hospital room. "It was 11 a.m.," she said, "and I could hear Jim speak. The doctor said, 'he's cured.'''
"They had never seen anything like this. He was so near gone," Ginger said, of the doctors and nurses. With the transfusion, "he was back to being Jim again." She had no hesitation in calling what had happened a "miracle."
Jim Warehime still has a long path to full recovery. Ginger said he's never far from the oxygen mask and uses a walker when he can. But, she said, the VA "remains our lifeline."
'You Can Come Through It'
"They told me I was a miracle, the first one at the Cleveland VA to come out of a coma and off the ventilator and survive," David James said.
When he awoke and was transferred to the intensive care unit, James said he could hear the nurses walking by and pointing: "There's the miracle patient."
His appearance testified to the ordeal. James said he lost 50 pounds while in treatment, shrinking from 265 to 215 pounds.
After leaving the Air Force, James said he worked for 39 years at the General Motors Lordstown plant near Youngstown, Ohio. He has worked a variety of jobs since, most recently as a school bus driver.
He's had a number of close calls over the years, including heart attacks, and said he had two carotid artery surgeries -- all treated at the VA. "The VA is the only place I go for medical care," he said.
He's not sure where he may have contracted the virus but said he began to feel out of sorts in March. On March 23, his wife, Patty, came home to find him listless in a chair.
"She asked where the dogs were, and I didn't know," James said.
"I'm taking you to the VA," she responded.
He said that he has "no memory whatsoever" of what took place between March 23 and April 15, shortly after the drug tocsilizumab was administered.
The recovery has been slow and difficult. The first time they tried to stand him up at the VA, he collapsed, James said. But he's now up to walking with a cane, sometimes as much as two miles.
"I'm still weak, memory's not back all the way," he said, but he has a powerful incentive for recovery: a Heritage Springer Classic motorcycle out in the garage.
Patty wasn't supposed to know about it but, yes, he's taken that hog back out on the road since he recovered. "I've been riding for 52 years," he said. "It's important to me."
His message to other veterans who fall victim to the virus: "there is hope. You can come through it, bad as it was."
'Blessing From God'
"How I got it, I'm not sure," said 20-year veteran airman Robert Colleton, originally from Yemassee, South Carolina.
He had underlying conditions, including a kidney transplant, that may have compromised his immune system and made him more susceptible to the virus, Colleton said. But he did not recall any symptoms until the first week of April, when he began experiencing a dry cough.
Even then, he did not feel particularly ill. But he called the VA at the Overton Brooks VAMC in Shreveport, Louisiana.
"They told me I probably need to come in," he said.
Colleton was tested for the virus and sent home to await results. A few days later, "I walked outside and I just collapsed. I guess I was pretty sick at the time."

Much like the other recovered veterans, Colleton said his memories of events at the hospital were a blur. He believes that at some point the doctors asked if he wanted to be put on a ventilator, and he agreed.
"I guess I was put on a ventilator, but I don't remember being put on it," he said. He also recalled thinking that he was "always cold and I could never sleep" during his stay at the VA. But he's not sure if that was really the case or "that was my mind playing tricks on me."
"I never understood what was happening to me," Colleton said, but in early May he awoke. He was taken off the ventilator. The doctors "told me how blessed I was. They told me I had survived and I was a fighter. I believe it had to be a miracle, a special blessing from God."
"I can't ever forget these people," he said of the staff at the VA. The illness left him with difficulties in motor coordination, and he now uses a walker.
"I was determined to walk again," he said.
'Hit Like A Bus'
"I thought this was the end," said Army Vietnam veteran and former New York Fire Department lieutenant Mike Bolnick.
The family had gone to a summer home near Harrison, N.Y., to lessen chances of catching the virus when New York City put shelter-in-place orders into effect.
On the fourth or fifth day after arriving, "I started to feel lousy," Bolnick said.
He thought he could sleep it off, "but I felt like I got hit by a bus. I thought I was dying. I knew something was wrong, but I had no idea I had the virus."
His wife, Dorothy, said, "Get up and get in the car." They first went to the Castle Point VA, part of the VA's Hudson Valley Heath Care System.
"I remember very, very little," Bolnick said. But he does recall somebody saying "he needs to be on a ventilator." That meant going to Albany Stratton VAMC, about 100 miles away.
He recalled little of the ambulance ride and nothing of his first 17 days at the hospital, when he was in an induced coma.
"The next thing I knew, it was a month later," Bolnick said.
When he awoke, "I didn't know my grandkids' names, who the president was. I couldn't even sit up. My cognitive ability was nil," but gradually "I started mentally coming back. I realized how fortunate I was."
"I thought Vietnam was tough, but this was a tough act," said Bolnick, who was a sergeant and squad leader with the 1st Cavalry Division, mostly operating in Tay Ninh province.
He was a New York City firefighter for 21 years after the war, rising to lieutenant and serving mostly with Ladder 27 in the South Bronx. He was retired when the planes hit the towers on Sept. 11, 2001. But, he said, you never really retire from NYFD. After the towers fell, he knew he had to help.
"You do what you have to do," Bolnick said.
He went down with the other retirees and volunteers to the wreckage of the World Trade Center to "work the pile." His two sons, Dustin and Michael, are now firefighters in the South Bronx.
Bolnick said he's still battling through the aftereffects of the virus. He's prone to headaches and fatigue, he said, and he has little strength in his right hand. At times, he can walk two miles, but "then I just want to lay down," he said.
Still, "I was better before I realized how close I was to dying."
He acknowledged that the VA has a somewhat checkered history on health care, and "there were [previous] times when I felt they fell short," but his current experience has changed his view.
"Every single person -- the doctors, the nurses, the staff -- were fantastic," he said.
-- Richard Sisk can be reached at Richard.Sisk@Military.com.
Related: The Military’s Coronavirus Cases: The Latest Rundown












